Management of latent tuberculosis infection
Introduction
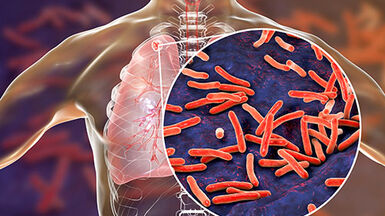
When people with infectious tuberculosis (TB) cough, sneeze or otherwise exhale droplets, they expose others to Mycobacterium tuberculosis. After a person is exposed, they can be infected with M. tuberculosis without having TB disease and without signs and symptoms. This is called latent TB infection (LTBI).
In people with LTBI, live TB bacilli remain inactive without causing disease, however the bacilli can at some point become active, multiply, and cause TB disease. The risk of progressing from LTBI to active TB disease is related to the virulence of the M. tuberculosis strain and the susceptibility of the host (e.g. malnutrition, immunocompromised status). People with LTBI represent a large human reservoir for TB, which is why management of LTBI is a crucial step towards TB elimination.
Around 60 000 cases of TB are reported annually in the European Union/European Economic Area (EU/EEA), with most countries in the region characterised by low-incidence of the disease (fewer than ten tuberculosis cases per 100 000 population). According to a recent estimate published in PLOS Medicine 1.7 billion people globally have LTBI - almost a quarter of the world’s population. In low incidence countries, a majority of TB cases occur due to the progression of LTBI from passive to active disease. This is why it is crucial to improve management of LTBI in Europe.
LTBI Management
To help decrease the incidence of LTBI, a variety of targeted public health measures need to be implemented.
It is crucial to identify groups at risk of contracting LTBI and those within the groups at risk of progressing to active TB. Identification of risk groups will enable targeted screening and treatment. Among the prioritised groups are people living with HIV, immunocompromised persons, patients with silicosis, people with pulmonary fibrotic lesions and contacts of infectious TB cases. Once the target groups are identified, defining a thorough diagnostic approach to detect LTBI is paramount. This approach should always involve screening with the tuberculin skin test and/or interferon gamma release assays. Detection of LTBI should be followed by treatment using a regimen based on an individual risk assessment and regular follow-up to ensure adherence.
Throughout the process, a culturally considerate and patient centred approach should be applied. This could include material incentives, counselling, education and peer-based support. Effective health education and communication should be maintained with target groups and healthcare providers concerning the importance of detecting and treating LTBI. To evaluate the suitability and effectiveness of LTBI management, reporting and monitoring procedures need to be implemented. Reporting systems should have adequate data collection processes, with defined performance indicators. National procedures should preferably be aligned with global and regional monitoring and evaluation frameworks, to enable country comparisons.