Examples of interventions to manage tuberculosis in vulnerable groups

Roma Health Assistants, Slovakia
In Slovakia, many tuberculosis cases occur among Roma people who live in disadvantaged settlements. To implement tuberculosis control programmes it was necessary to better engage with the Roma community.
The solution was to identify Roma health assistants, key persons in the community that serve as mediators.
Roma Health assistants are community workers, living in the settlement they’re covering. They monitor patients’ treatments, do contact tracing, accompany patients to doctor’s appointments, ensure that the patients get their TB drugs, and keep record of all activities and interventions.

The assistants know how to talk to people from the communities and are well accepted. For example they don’t push people, if needed they ask for help from family members who have influence over the patient, they take into account that health is not perceived as a priority, and explain the importance of taking the medication not only to get better, but also to avoid dying.
The assistants receive regular training, tailored to their needs and the specificities of the community they are covering. Topics range from basic first-aid to epidemiology. They are trained specifically for TB care and can recognise symptoms, know the mode of transmission, treatments and drugs side-effects.
Outcome
As a result of the Roma assistant programme, more than 80% of adult Roma people with TB have been successfully treated in Slovakia. In addition, TB outbreaks have been promptly identified and contained and all index cases for children’s TB cases have been identified.
The Health assistant programme was launched in 2007 and by the end of 2015, 288 health assistants and coordinators were covering two thirds of the Roma population settlements. It is planned to develop the programme further and to cover all Roma communities.
Key elements to the success of this intervention:
- Selecting assistants from the same communities;
- Providing training of high quality, and continuously adapting the training programmes based on the assistants’ needs;
- Ensuring good cooperation and communication between the Roma Health Assistant and all local health care providers (general practitioners, paediatricians, district TB specialist, hospital staff);
- Adequate funding of the programme to ensure decent salaries and working conditions for the health mediators.

Eduard’s story
Eduard is married, he has three children and 12 grandchildren, they all live in Roma settlements in eastern Slovakia.
In summer 2015 he was diagnosed with tuberculosis by a local general practitioner (GP). He was hospitalised for a month and when he was released, a Roma Health assistant was assigned to ensure the follow-up care. The Assistant arranged for daily Directly Observed Treatment (DOT), he checked for treatment side-effects, he accompanied Eduard to his medical appointments and arranged visits to the local pharmacy to pick-up medications.
The Health assistant also helped with contact tracing to identify if other people were infected with TB. Finally, eighty-six contacts were identified and went through screening, including his wife, children and grandchildren. They were all negative but his grandchildren received a prophylactic treatment. Throughout the children’s hospital visits, the Health Assistant served as communication link between the hospital staff and the family.
Eduard’s health has improved and he’s still taking his treatment against TB. Thanks to the help of Milan, his Roma Health Assistant, he has learned a lot about TB. ‘It is important that people with TB take their medicines even after they start to feel better. Because only if they finish their medicine they will survive! TB treatment helped me to cheat death!’ he said.

Video Observed Treatment, UK
Directly Observed Treatment (DOT) is a method to assist patients so they complete their treatment. It is proposed to patients with severe variants of tuberculosis or to those who might face difficulties with taking their medication. It includes providing and watching the patient swallow the medication, checking for side-effects, and informing the patient about the disease.
The London based outreach team of Find&Treat was established to find cases of tuberculosis among vulnerable groups. Now they also make sure that the identified patients take the full course of their treatment. For that, depending on the needs of the patients, they set up either DOT or another option: the Video Observed Treatment (VOT).
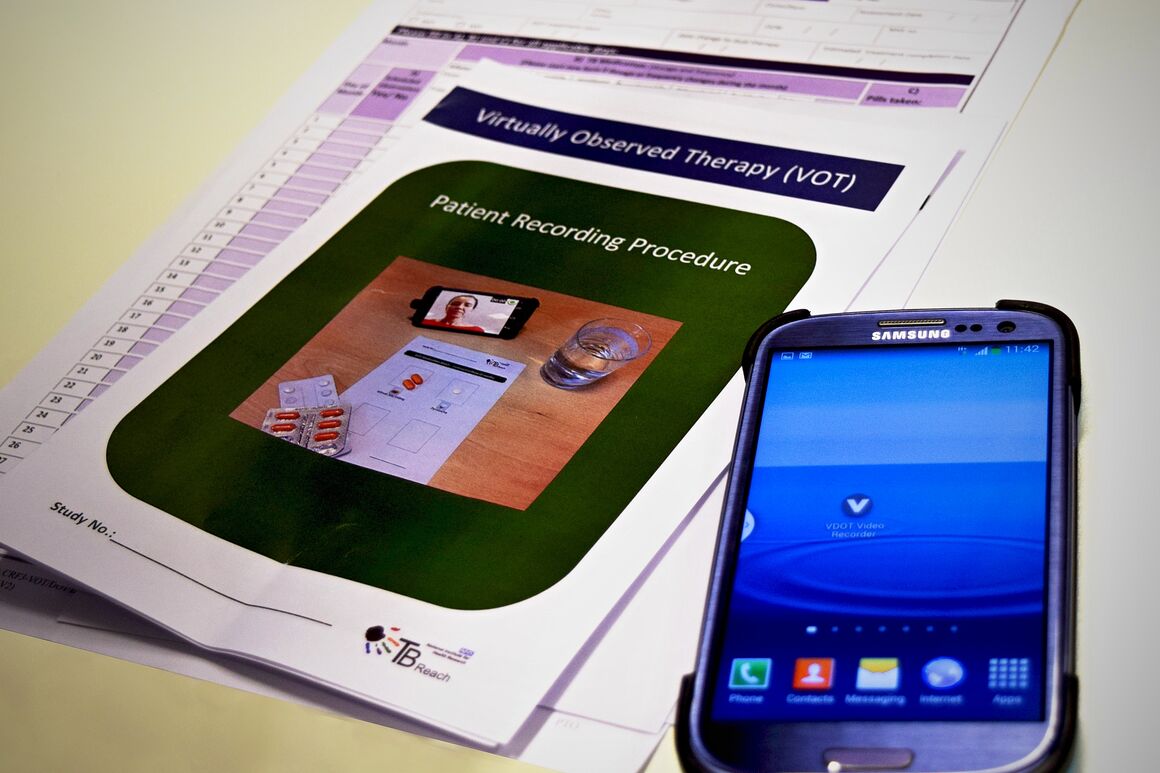
Patients selected for VOT first receive face-to-face instructions from the person who will monitor the videos and do the follow-up. Thereafter, they will film themselves while taking their pills and submit the videos. They can also report side-effects and ask questions in the videos.
The video monitors screen the videos to verify whether the protocol is followed, send reminders, answer queries and provide support when needed.
As internet access is crucial to the success of this intervention, some patients are provided with a smartphone and/or data package. This functions as an incentive and also facilitates the communication between the patients and healthcare services, for example to set-up appointments and to send reminders.
Main advantages of the VOT alternative compared to DOT:
- For the patient: more flexibility on when/where to take medication, saves time, improves confidentiality, and gives a more active role in own treatment.
- For healthcare services: saves money, increases productivity (more patients can be covered in less time), reduces exposure of healthcare workers to TB.

Gitanas’ story
Gitanas comes from Lithuania and moved to London in 2010 to find a better life. During his stay in shared housing, one of the lodgers was coughing a lot. Later, Gitanas and four others in the house were diagnosed with multidrug-resistant TB (MDR TB). As Gitanas had to stay in the hospital for six weeks for the initiation of his tuberculosis treatment, he couldn’t work and pay the rent, so he lost his flat.
He was referred for Directly Observed Treatment (DOT) by the hospital and then for Video Observed Treatment (VOT). It was the team from Find&Treat who recommended his transfer, given his intensive treatment (27 pills, 3 times a day), lack of housing and employment. In September 2013 Gitanas started his VOT with Find&Treat.
Despite serious side-effects of the medication that made him feel sometimes worse, Gitanas hold on to the VOT routine and sent films every day for two years. ‘At the beginning I thought this is all very strange, why are they asking me to do this? But after a while I understood this was to help me finish with the tuberculosis. I took tablets three times a day and the VOT helped me to get into a rhythm. It was part of the job of getting better’ he said.
VOT helped Gitanas to keep going, providing virtual support, advice and encouragement. Gitanas successfully completed his treatment in July 2015.

Outreach TB team, France
The Samusocial is an emergency service of the city of Paris, which provides help and ambulatory medical care to homeless people. In 2000, a specific mobile unit was created: the TB outreach team EMLT (Equipe Mobile de Lutte contre la Tuberculose). Its purpose is to find TB patients and support them to complete their treatment.
The EMLT is a multidisciplinary team of nine people (nurses, pneumologist, social worker, drivers, administrator), with two vans, and a very large network of partners providing social, health, legal services such as accommodation structures with nursing beds, drug and alcohol rehabilitation centres etc. Once a TB patient is referred to EMLT, the team visits the patient wherever he or she is, in hospital, sanatorium, shelter, or on the street. Over the years, EMLT has learned how to find people, using their extended network to find out people’s routines and territories.

The EMLT approach is respectful and supportive. ‘Each patient has a different struggle’ said Dr Rivoire, EMLT medical director. ‘We know that people have many concerns and TB is just one and not always the most pressing. While our underlying aim is to get people take their medicine, we know we need to deal with the issues people see as most important to their lives first’ she added.
Core features contributing to the success of EMLT:
- Patient’s care beyond the treatment of TB: ensuring people’s basic needs such as food, clothing and shelter are covered, adapting solutions to each patient’s specific situation, helping them with longer term life planning;
- Extensive formal and informal support network: facilitating access to community-based accommodation structures with nursing beds, putting patients in contact with the relevant social, health and legal agencies;
- Mobile capacity of a multidisciplinary team: operating outside healthcare facilities, finding and following-up patients wherever they are (shelters, hospitals, on the streets), combining various perspective and experience to better understand each patient.

Sathees’ story
Sathees originates from Sri Lanka, he arrived in Paris in 2011 without job nor papers. He was living on the streets and was drinking heavily.
Sathees was sick for several months until he got diagnosed with TB. Early 2014, he was transferred to the TB sanatorium for severe cases. The outreach TB team EMLT (Equipe Mobile de Lutte contre la Tuberculose) was called in to help managing Sathees’ case. His treatment was especially challenging because of his alcohol problem. Sathees left the sanatorium several times to go back on the streets of Paris to his drinking habit. Every time, the staff called the EMLT team who always managed to find him and to convince him to return to treatment.
Over the course of his eight month stay at the TB sanatorium, the EMLT staff helped him to stop drinking and gave him the opportunity to attend French classes, as he wanted to stay in France.
When Sathees was discharged, the EMLT team helped him to find a shelter with nursing care and to successfully complete his full treatment. ‘I like the people in France. They took care of me in the hospital and are continuing to help me with temporary accommodations while I apply for asylum and get my papers sorted’ he said. ‘EMLT has helped me think for myself and stop being negatively influenced by others around me.’ he concluded.
Scientific and technical publications
Interventions in vulnerable groups are the key to eliminating tuberculosis in Europe
Tuberculosis (TB) is a serious infectious disease that although treatable, can be fatal. In 2014, it affected around 58 000 people in the European Union/European Economic Area (EU/EEA). This short document gives an overview of why interventions among vulnerable groups are necessary and what can be done, with examples and data to give evidence of the points raised.