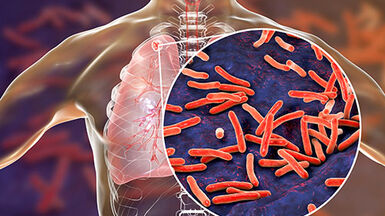
Facts about tuberculosis
Tuberculosis (TB) is a severe infectious disease caused by various strains of mycobacteria, most commonly Mycobacterium tuberculosis. TB affects the lungs (pulmonary tuberculosis), but can also manifest outside the lungs (extrapulmonary tuberculosis). People are infected with TB by inhaling airborne droplets produced by infectious TB carriers - for example when coughing or sneezing. Latent tuberculosis infection (LTBI) carriers are asymptomatic and not infectious. About 10% of those with LTBI develop active TB.
Tuberculosis symptoms vary depending on the affected area. Pulmonary TB is characterised by a cough with sputum (sometimes with blood), chest pain, shortness of breath and a general feeling of weakness. Extrapulmonary TB can affect any part of the body and symptoms are site-related.
The BCG (Bacillus Calmette–Guérin) vaccine provides partial protection against TB. Standard treatment of TB consists of a six-month regimen of four first-line drugs (isoniazid, rifampicin, ethambutol and pyrazinamide). Multidrug-resistant (MDR) and extensively drug-resistant (XDR) TB require longer treatment with at least five drugs and have a higher fatality rate.
European context
In the European Union and European Economic Area (EU/EEA), tuberculosis (TB) rates are among the lowest in the world, with less than 60 000 cases reported annually. The EU/EEA notification rate has experienced a downward trend since the launch of European-enhanced TB surveillance in 1996. There is marked variation between countries in the number of cases reported, with country-specific notification rates differing more than 20-fold. Three countries (Poland, Romania and the United Kingdom) account for roughly 40% of all reported cases, with Romania alone accounting for approximately 20%. Estonia, Latvia and Lithuania have the highest rate of multidrug-resistant (MDR) TB; more than 10% of the TB cases reported are diagnosed with MDR TB in these countries. In low-incidence countries, there are significant inequalities in TB rates among population subgroups, while in countries with a higher incidence, TB affects all population groups.
Common challenges
Timely detection and correct diagnosis
Early detection of TB is important to prevent further transmission. Diagnosis is often delayed for TB, which can be due to multiple factors: lack of knowledge of the disease in low-incidence settings, non-specific symptoms (especially in the case of HIV co-infection and extrapulmonary TB), and inadequate access to healthcare for vulnerable groups.
Completion of treatment
Completion of treatment is important to cure patients and prevent transmission. TB treatment involves taking a combination of drugs for several months. The treatment often causes side-effects and can be costly. Unfinished treatment or non-compliance to the prescribed treatment is problematic as it can lead to drug-resistance. TB patients often face difficulties in adhering to treatment and therefore require patient-centred support to enable them to follow a full course of treatment.
Multidrug-resistant (MDR) and extensively drug-resistant (XDR) TB
Variants of TB that are resistant to antibiotics are more difficult and expensive to treat, and have higher fatality rates. Their spread is a major challenge to the elimination of TB.
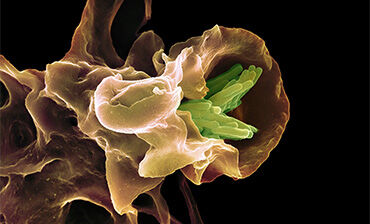
Latent tuberculosis infection
In people with latent tuberculosis infection (LTBI), live TB bacilli remain inactive without causing disease, however the bacilli can at some point become active, multiply, and cause TB disease. People with LTBI represent a large human reservoir for TB, which is why management of LTBI is a crucial step towards TB elimination.