Factsheet on A(H5N1)
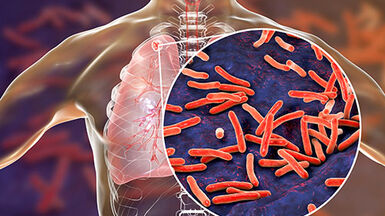
Highly pathogenic avian influenza virus A(H5N1)
Avian influenza viruses can cause infection in birds and humans. The classification of avian influenza viruses as ‘low pathogenic’ or ‘highly pathogenic’ is defined either by the composition of the cleavage site in the haemagglutinin (HA) gene or by the intravenous pathogenicity index in six-week old chickens in accordance with the criteria listed in Council Directive 2005/94/EC and the OIE International Health Standards. Highly pathogenic avian influenza viruses (HPAIV) cause high mortality in infected chicken, while low pathogenic viruses (LPAIV) result in mild disease or asymptomatic infection.
HPAIV A(H5N1) is highly infectious for a number of bird species, including most species of domestic poultry [1]. Unlike most other avian influenza viruses, this virus has also infected mammals, including cats, pigs and tigers, and has shown to be able to transmit to humans. However, the virus remains poorly adapted to humans, and transmission from birds to humans is a rare event [2]. Since the first detection of zoonotic transmission of HPAI A(H5N1), limited clusters of human cases have occurred but no sustained human-to-human transmission has been observed but showed. Zoonotic transmission to humans from infected birds occurs either directly or through environmental contamination. Hence, almost all human infections have been related to close contact with infected or sick birds or their faecal products in domestic settings, e.g. in ‘wet markets’ in Asia or in backyard farming [3]. The circulation of HPAI A(H5N1) in bird populations in different regions of the world has contributed to the emergence of different virus clades [4].
Case definition
All human cases infected with a novel influenza strain are notifiable in the EU under EU legislation and the International Health Regulations (IHR) through the Early Warning and Response System (EWRS) and IHR, respectively. Human infections with A(H5N1) are notifiable according to EU Decisions 2018/945 and 1082/2013/EU.
All infections in poultry caused by avian influenza virus (AIV) of any subtype fulfilling the in vivo criteria for high virulence laid down in the Terrestrial Animal Health Code of the World Organisation for Animal Health (OIE), The detection and control of avian influenza in the EU/EEA is laid down in the Animal Health Law adopted in the Regulation (EU) 2016/429.
Case definition: Avian influenza A(H5) OR A(H5N1) in humans
Clinical criteria
Any person with one of the following two:
— Fever AND signs and symptoms of acute respiratory infection
— Death from an unexplained acute respiratory illness
Laboratory criteria
At least one of the following three:
— Isolation of influenza A(H5N1) from a clinical specimen
— Detection of influenza A(H5) nucleic acid in a clinical specimen
— Influenza A(H5) specific antibody response (fourfold or greater rise or single high titre)
Epidemiological criteria
At least one of the following four:
— Human-to-human transmission by having been in close contact (within one metre) to a person reported as probable or confirmed case
— Laboratory exposure: where there is a potential exposure to influenza A(H5N1)
— Close contact (within one metre) with an animal with confirmed A(H5N1) infection other than poultry or wild birds
(e.g. cat or pig)
— Reside in or have visited an area where influenza A(H5N1) is currently suspected or confirmed* AND at least one of the following two:
-- Having been in close contact (within one metre) with sick or dead domestic poultry or wild birds** in the affected area
-- Having been in a home or a farm where sick or dead domestic poultry have been reported in the previous month in the affected area
Case classification
A. Possible case
Any person meeting the clinical and the epidemiological criteria
B. Probable case
Any person with a positive test for influenza A(H5) or A(H5N1) performed by a laboratory which is not a National Reference Laboratory participating in the EU Community Network of Reference Laboratories for human influenza (CNRL)
C. Nationally confirmed case
Any person with a positive test for influenza A(H5) or A(H5N1) performed by a National Reference Laboratory participating in the EU Community Network of Reference Laboratories for human influenza (CNRL)
D. WHO confirmed case
Any person with a laboratory confirmation by a WHO Collaborating Centre for A(H5)
* See World Organisation for Animal Health (OIE) and the European Commission’s Animal Disease Information System (ADIS), available from: https://www.oie.int/en/what-we-do/standards/codes-and-manuals/terrestrial-code-online-access/ and https://ec.europa.eu/food/animals/animal-diseases/not-system_en
** This does not include seemingly well birds that have been killed, for example by hunting.
Pathogen
Since 1996, when HPAI A(H5N1) virus was first observed in China, detections in wild birds and poultry have been reported worldwide and recorded in a WHO timeline. Since its first detection, HPAI A(H5N1) has evolved, resulting in multiple genetic lineages (clades) across the world and human cases are related to different clades and subclades (https://pubmed.ncbi.nlm.nih.gov/32686602/).
Various influenza A(H5) subtypes, such as influenza A(H5N1), A(H5N2), A(H5N3), A(H5N4), A(H5N5), A(H5N6) and A(H5N8) have been detected in birds in Europe (see joint ECDC/EFSA/EURL avian influenza situation reports). Although these influenza A(H5) viruses might have the potential to cause disease in humans, only sporadic human cases of infection due to A(H5N1), A(H5N6) and A(H5N8) viruses have been reported so far (Scientific report Art_31_ AI monitoring_March 2019 (europa.eu)).
Epidemiology
Detections of HPAI A(H5N1) in poultry and wild birds were initially reported in the Far East, and later, in parts of Europe, the Middle East, Africa and the United States (as listed by FAO).
In 1997, Hong Kong identified the first human infections. In 2003, the first confirmed human cases were notified by WHO, and since then more human cases and fatalities have been reported by WHO (see detailed timeline).
Between 2003 and 2017, high numbers of human cases were reported from 17 countries worldwide, since 2018 only a few sporadic cases have been reported, none from the EU/EEA (See Avian Influenza Overviews). In December 2021, a mild A(H5N1) infection in a person above 75 years of age that had close exposure to infected ducks was reported from the United Kingdom . Other zoonotic transmission events have been reported in cats, foxes, otter, pigs and mustelids (See Avian Influenza Overviews).
Clinical features
The clinical course of human cases of A(H5N1) is characterised by initial fever and cough, with rapid progression to lower respiratory disease. Upper respiratory tract symptoms of rhinorrhoea and sore throat might not be common in all patients, but the disease can progress to respiratory failure, acute respiratory distress syndrome (ARDS) and multi-organ failure [5].
The overall case–fatality ratio (CFR) is around 50%, although this appears to differ from country to country. The CFR has been lower in Egypt, which may be due to a lower virulence of the virus clade and the early detection as well as better treatment of human cases. Indonesia has reported the highest number of fatal cases overall, with a CFR of 84%.
Transmission
The incubation period for A(H5N1) infection has been estimated to be up to seven days, although it is usually two to five days after the last known exposure to sick or dead poultry. Longer periods have, however, been suggested [5].
A subset of avian influenza viruses may infect humans; whenever such viruses are circulating in poultry, sporadic infections or small clusters of human cases are possible in people exposed to infected poultry or contaminated environments, especially related to backyard settings. Human infections remain rare, and influenza A(H5N1) viruses do not appear to transmit easily between people.
Small clusters with the same exposure prior to disease onset have been observed, yet no sustained human-to-human transmission has been identified. Human cases have reported direct exposure to apparently healthy looking or sick poultry, mostly backyard poultry before onset of disease. The most commonly identified risk factors associated with A(H5N1) virus infection include contact with infected blood/organs or bodily fluids of infected poultry through food preparation practices; touching and caring for infected poultry; exposure to A(H5N1) by swimming or bathing in potentially virus-laden ponds, exposure to A(H5N1) at live bird markets in Asia and via backyard poultry in Egypt [3].
Diagnostics
EU legislation for the detection and control of avian influenza in the EU/EEA is laid down in the Animal Health Law adopted in the Regulation (EU) 2016/429.. This legislation specifies in detail the detection and diagnosis of H5 viruses in birds.
No EU legislation for human cases in Europe exists. Risk management is managed under the authority of Member States.
People in the EU presenting with severe respiratory or influenza-like infection and a history of exposure to poultry or wild birds will require careful investigation, management and infection control. Appropriate samples for influenza tests should be rapidly taken and processed from patients with relevant exposure history within ten days preceding symptom onset. If positive specimens cannot be subtyped, those should be shared with the national reference laboratory (National Influenza Centres; NICs).
With routine diagnostic laboratory assays, human infection with A(H5Nx) viruses should be detected as positive for influenza A virus, and negative for influenza B, A(H1), A(H1)pdm09 and A(H3) viruses and therefore classified as un-subtypable influenza A virus if no-specific A(H5) diagnostic test is performed. Such un-subtypable influenza A virus isolates or clinical samples that cannot be subtyped should be sent to NICs, and further to a WHO Collaborating Centre for Reference.
Case management and treatment
WHO has published guidance on the clinical management of human infection with A(H5N1) as well as rapid advice guidelines on pharmacological management of humans infected with avian influenza A (H5N1) virus, which contains a chapter on ‘chemoprophylaxis of H5N1 infection’.
Four licensed influenza antiviral agents are available in the EU/EEA: amantadine, rimantadine, zanamivir and oseltamivir. However, current circulating seasonal influenza A viruses are resistant (>99%) to the adamantanes (amantadine and rimantadine). Isolates of influenza A(H5) strains are also widely resistant to the adamantanes [6]. Zanamivir and oseltamivir are included in a class of drugs known as influenza neuraminidase inhibitors and are active against both influenza A and B viruses. Baloxavir marboxyl (Xozaflu) has been authorised in 2020 in the EU/EEA.
HPAI A(H5N1) viruses have so far been reported to be sensitive to neuraminidase inhibitors, even though a few viruses of the Egyptian clade showed resistance.
Public health control measures
Given the potential zoonotic risk, contingency plans for the control of avian influenza in poultry and birds should be considered. Public health and occupational health authorities need to make sure that persons at risk are sufficiently protected from infection.
In Europe, persons directly exposed to the virus or close contacts of confirmed cases should be considered for follow-up by the local health service to identify human-to-human transmission events.
Evidence of the effectiveness of contact tracing of airplane passengers in reducing the spread of the infection is limited and should only be considered after conducting a risk assessment on a case-by-case basis as outlined in the ECDC risk assessment guidelines for infectious diseases transmitted on aircraft (RAGIDA).
Surveillance systems for early disease detection to monitor new introductions have been established. The animal health control mechanisms to control outbreaks of avian influenza are laid down in the Animal Health Law. Main measures are the culling of birds in the affected holdings.
Infection control, personal protection and prevention
Appropriate personal protective equipment, including respiratory protection, should be made available and used during outbreaks. All protective equipment should meet national guidelines and regulations.
People unprotected and directly exposed to infected birds should be monitored for 10-14 days in order to document possible related symptoms. As a minimum, exposed people should self-monitor and report any respiratory symptoms or conjunctivitis to local health authorities, mentioning their previous exposure to be tested as soon as possible. Local health authorities may consider ways to actively monitor these groups and administer antiviral prophylaxis dependent on the local risk assessment (i.e. intensity of exposure).
Unvaccinated persons that are exposed to avian influenza viruses as a result of their occupation should be offered vaccination against seasonal influenza in accordance with national guidelines.
Candidate vaccine viruses against different H5 clades are currently under development and are regularly updated during the Vaccine Composition Meetings at WHO twice a year.
Advice to travellers
Travel-associated cases were detected in Canada and Malaysia, but no cases of A(H5N1) among EU travellers have been reported. Travellers should be advised to avoid direct contact with poultry or poultry products in affected countries.
References
1. Kelly TR, Hawkins MG, Sandrock CE, Boyce WM. A review of highly pathogenic avian influenza in birds, with an emphasis on Asian H5N1 and recommendations for prevention and control. J Avian Med Surg. 2008 Mar;22(1):1-16.
2. Malik Peiris JS. Avian influenza viruses in humans. Rev Sci Tech. 2009 Apr;28(1):161-73.
3. Van Kerkhove MD, Mumford E, Mounts AW, Bresee J, Ly S, Bridges CB, et al. Highly pathogenic avian influenza (H5N1): pathways of exposure at the animal-human interface, a systematic review. PLoS One. 2011;6(1):e14582.
4. World Health Organization/World Organisation for Animal HF, Agriculture Organization HNEWG. Revised and updated nomenclature for highly pathogenic avian influenza A (H5N1) viruses. Influenza Other Respir Viruses. 2014 May;8(3):384-8.
5. Uyeki TM. Human infection with highly pathogenic avian influenza A (H5N1) virus: review of clinical issues. Clinical Infectious Diseases. 2009 Jul 15;49(2):279-90.
6. Dong G, Peng C, Luo J, Wang C, Han L, Wu B, et al. Adamantane-resistant influenza a viruses in the world (1902-2013): frequency and distribution of M2 gene mutations. PLoS One. 2015;10(3):e0119115.
7. European Medicines Agency. CHMP scientific opinion 2010. London: EMA; 2010.
8. European Medicines Agency. Adjupanrix (previously Pandemic influenza vaccine (H5N1) (split virion, inactivated, adjuvanted) GlaxoSmithKline Biologicals) 2013 [cited 2015 26 August].
9. European Medicines Agency. Prepandemic influenza vaccine (H5N1) (surface antigen, inactivated, adjuvanted) Novartis Vaccines and Diagnostics 2011 [cited 2015 26 August.
10. European Medicines Agency. Pandemic Influenza Vaccine H5N1 Baxter AG 2014 [cited 2015 26 August].