Facts about avian influenza in humans
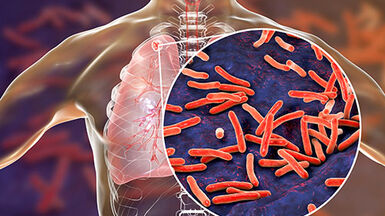
Influenza is an infectious disease that primarily presents with respiratory signs and symptoms, caused by RNA viruses. The most significant impacts of influenza viruses on humans are those arising from the influenza A strains. The natural reservoir of influenza A strains is a diverse pool of viruses among aquatic wild bird populations – the avian influenza (AI) viruses. These viruses are of high pathogenicity (HPAI) and low pathogenicity (LPAI), according to their severity in the avian species they usually infect. HPAI epizootics have been documented worldwide due to the A/H5 and A/H7 virus groups. The ongoing A/H5 outbreaks in wild and farmed birds are affecting several countries worldwide, and have caused sporadic transmission events to humans.
Most cases of avian influenza in humans have been due to transmission from birds, but there have also been events when the transmission has been from other sources, for e.g. from contaminated environment. Millions of wild or farmed birds have died in huge epizootics, either directly from the infection or from subsequent culling measures undertaken to control the infection. Since the 2019/2020 epidemic period, there have been larger and more frequent outbreaks of HPAI in wild birds and poultry than previously experienced in Europe . The reason for this is unknown. Both large and small outbreaks have occurred in Europe due to different avian influenza virus subtypes.
Read more: Avian influenza overview: Latest situation update of the avian influenza situation in EU/EEA
There are two forms of risk to the health of humans from avian influenza viruses:
- There is risk from infection by the native form of the avian influenza virus.
- There is also risk posed by the potential for the emergence of new pandemic strains either directly from avian influenza viruses, or from their recombination with human or other animal viruses.
The ‘high’ and ‘low’ pathogenicity of avian influenza viruses is not related to the disease in humans. Some avian viruses do not cause disease in humans, or are known to only cause mild disease. Others, however, are known to cause severe disease in humans, for example, the influenza A virus subtype A(H5N1). The classification of avian influenza viruses as ‘low pathogenic’ or ‘highly pathogenic’ is defined either by the composition of the cleavage site in the haemagglutinin (HA) gene, or by the intravenous pathogenicity index in six-week-old chickens in accordance with the criteria listed in ‘Animal Health Law’ and the WOAH Terrestrial Code .
Any detection of avian influenza viruses of the H5 and H7 subtypes in birds needs to be notified. Following which, precautionary measures are adopted to prevent potential avian-to-human infection.
A(H5N1)
The avian influenza virus A(H5N1) emerged in 1996. It was first identified in southern China and Hong Kong. The A(H5N1) virus kills a high proportion of the poultry that it infects, and is therefore known as a highly pathogenic avian influenza virus. It remains poorly adapted to humans. Transmission from birds to humans is infrequent and no sustained human-to-human transmission has been observed. However, it can cause severe disease in humans.
The A(H5N1) virus has only been sporadically detected in European poultry or wild birds until 2021. Since then, A(H5N1) has caused the largest outbreaks in wild and farmed birds ever observed in Europe. It has affected more than 50 million birds during the 2021/2022 epidemic alone.
A(H7N9)
A novel avian influenza A virus, A(H7N9), was identified in China in March 2013, causing severe illness in humans. This was the first time that a low pathogenic avian influenza A virus was associated with fatal outcomes for humans. This subtype has developed into a highly pathogenic form which also causes human infections. Following mass vaccinations of poultry in China, only sporadic human infections have been observed, with the last case reported in March 2019
Influenza virus detections in poultry in EU/EEA
In 2014/2015, a highly pathogenic avian influenza virus subtype, A(H5N8) was introduced into Europe. Outbreaks in poultry and detections in wild birds were notified by several European countries.
Previously, this virus was detected among wild and poultry in Asia. A large epidemic followed in the period 2016/2017. Until the end of 2019, only sporadic detections and outbreaks were observed due to A(H5N8) when then again large outbreaks mostly during the winter period were observed. Since 2019, a larger global spread was observed along with the emergence of highly diversified viruses. This was also due to reassortment with local subtypes. This led to a shift of the dominant virus subtype from A(H5N8) to A(H5N1) in 2021. Also, a large number of different wild bird species were affected leading to unprecedented large outbreaks in colony-breeding birds during the summer of 2022. This caused the circulation of highly pathogenic avian influenza viruses in wild birds year-round in Europe. In 2022, highly pathogenic avian influenza viruses of the A(H5N1) subtype were introduced into North America through migratory birds and further into Middle and South America, which had never reported any A/H5 viruses.
Read more:
Situation reports at World Organisation for Animal Health
Avian influenza overview: Latest situation update of the avian influenza situation in EU/EEA
Ongoing monitoring and testing of wild and farmed birds in the EU are important to detect and prevent the further spread of this highly pathogenic virus to humans.
Human exposure and infections in the EU/EEA
In the past, outbreaks of highly pathogenic avian influenza viruses have mostly affected poultry farms in the EU/EEA. The required control measures involve the culling of infected birds and cleaning of affected premises, which is often performed by specific culling and cleaning teams with the due observance of safety measures including the use of personal protective equipment. However, more recently, outbreaks in backyard flocks or other settings with captive birds as well as in wild birds have also required control measures that led to a large number of single-exposure events. For the period, 2016–18 more than 10 000 single-exposure events were estimated to have occurred in the EU/EEA, mostly related to large commercial farms, but also due to outbreaks in smaller commercial and non-commercial settings. (Estimation of the number of exposed people during highly pathogenic avian influenza virus outbreaks in EU/EEA countries, October 2016–September 2018 - PMC (nih.gov))
Since 2020, the largest epidemics of avian influenza in wild birds and poultry have been observed, leading to more than 50 million dead birds and culled poultry in 2021/2022 alone. Highly pathogenic avian influenza viruses have caused high morbidity and mortality in different wild bird species leading to mass mortality events in colony-breeding sea birds. All these outbreaks required human involvement and therefore, humans were exposed to infected or potentially infected birds either in poultry farms, zoos, hobby flocks, urban or rural areas.
Despite the large number of human exposure events caused in response to the outbreaks in poultry farms (culling, cleaning and other control measures as well as wild bird findings), no avian influenza virus infection causing illness was observed in the EU/EEA countries. In 2022, Spain reported two asymptomatic workers involved in culling and cleaning who tested positive for A(H5N1), but were considered as having contaminated nasal mucosa due to very low virus load identified in PCR tests, the inability to cultivate virus and no antibodies to A/H5.
Similar cases were reported from other countries such as the United Kingdom and the United States, where PCR tests amplified A/H5 fragments in exposed people without or with only very mild symptoms.
Transmission of avian influenza viruses to humans are rare events but need to be identified as soon as possible to implement follow-ups of contact persons and other public health measures to investigate any possible human-to-human spread. Persons at risk are mainly those in direct contact/handling diseased birds or poultry, or their carcasses (e.g. farmers, veterinarians and labourers involved in the culling and rendering), as well as those exposed to contaminated environments.
Questions and answers on avian influenza
What is avian influenza (bird flu)? Why are we concerned about bird flu outbreaks? What are the control measures in birds and animals? How do outbreaks of avian influenza spread?