Factsheet about meningococcal disease
Meningococcal disease is caused by the bacterium Neisseria meningitidis. The bacterium is often detected in the nasopharynx without causing disease, a situation described as asymptomatic carriage. The bacteria occasionally invade the body and cause meningococcal infection, which is an acute severe bacterial infection. Invasive meningococcal disease (IMD) is a major cause of meningitis and septicaemia.
The disease often has a rapid progression, with an 8–15% case-fatality ratio. The highest incidence occurs in young children, with a second disease peak among adolescents and young adults. IMD is notifiable and under surveillance in EU/EEA countries.
Outbreaks of meningococcal disease are rare, but can occur in settings where people group together, such as college campuses and military recruits. Vaccines are available for primary prevention of disease caused by serogroups A, B, C, W, and Y. Antibiotics are available for elimination of carriage and treatment of disease.
Case definition
All Member States use the EU case definition (Commission Implementing Decision 2012/506/EU of 8 August 2012 of the European Parliament and of the Council) or a case definition compatible with the EU case definition for confirmed cases.
Clinical criteria
Any person with at least one of the following symptoms:
- meningeal signs
- haemorrhagic rash
- septic shock
- septic arthritis
Laboratory criteria
At least one of the following:
- isolation of Neisseria meningitidis from a normally sterile site or purpuric skin lesions
- detection of Neisseria meningitidis nucleic acid from a normally sterile site or purpuric skin lesions
- detection of Neisseria meningitidis antigen in cerebrospinal fluid (CSF)
- detection of gram-negative stained diplococcus in CSF
Epidemiological criteria
An epidemiological link by human-to-human transmission.
Case classification
A. Possible case
Any person meeting the clinical criteria.
B. Probable case
Any person meeting the clinical criteria and with an epidemiological link.
C. Confirmed case
Any person meeting the laboratory criteria.
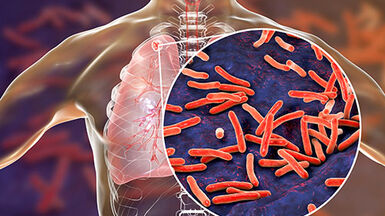
Pathogen
Neisseria meningitidis is a gram-negative diplococcus. Based on structural differences of the polysaccharide capsule, bacteria are classified into serogroups, of which eight are most commonly reported from invasive infections: A, B, C, X, Y, Z, W135 and L. Multilocus sequence typing of seven housekeeping genes is used to categorize Neisseria meningitidis into different sequence types and clonal complexes. The key virulence factor is the polysaccharide capsule that surrounds the outer membrane, which helps bacteria resist phagocytosis and complement-mediated lysis. Genomic technologies have revealed a limited range of hypervirulent lineages with a higher likelihood of association with invasive disease, which tend to partition into geographical regions. Emerging clones can cause explosive epidemics and spread rapidly within countries and internationally.
Clinical features and sequelae
Meningitis (30–60%) and sepsis (20–30%) are the major clinical features of IMD. Less common are other focal diseases such as pneumonia and arthritis. Meningitis frequently presents with the triad of fever, headache and neck stiffness, and is often accompanied by other symptoms, such as altered mental status, nausea, vomiting and photophobia. Meningococcal sepsis (meningococcemia) is characterised by fever and a petechial or purpuric rash, often accompanied by septic shock, disseminated intravascular coagulation and multiple organ failure. Meningococcemia has a case-fatality ratio of up to 40%. Sequelae such as neurological and hearing impairment or amputation occur in up to 20% of survivors.
Epidemiology
Information on the incidence of invasive meningococcal disease in the EU/EEA is presented in the ECDC annual epidemiological report.
Transmission
Humans are the only reservoir of Neisseria meningitidis. Transmission occurs by droplet aerosol or secretions from the nasopharynx of colonised persons. The average incubation period is 3–4 days (usually ranging from 2–10 days). An upper limit to the incubation period is unknown. The infective period effectively stops within 24 hours after the initiation of appropriate antibiotic therapy. The administration of antibiotics to close contacts is recommended as a control measure.
Diagnostics
The diagnosis of IMD is based on bacteriologic isolation, antigen or DNA detection of Neisseria meningitidis in a usually sterile body fluid such as blood, CSF or synovial or pleural fluid. The sensitivity of culture is reduced after the initiation of antimicrobial therapy and polymerase chain reaction-based assays are increasingly used for the diagnosis of meningococcal disease. Microbiological confirmation is necessary to fulfil the case definition of a confirmed case according to the EU case definition.
Case management and treatment
Prompt recognition of disease and administration of antibiotics, usually beta-lactam, are vital to improve the outcome in IMD.
Options for contact management of sporadic cases of IMD is illustrated in an ECDC guidance. However, this may differ according to setting and context and national/regional guidances available in the EU/EEA should be consulted.
Public health control measures
Advances in the control of meningococcal disease have taken place over the past decades through prophylactic vaccination. Vaccination against IMD is part of general immunisation programs in certain EU/EEA Member States, while other countries only recommend the vaccination of specific risk groups.
All licensed meningococcal vaccines are inactivated. There are polysaccharide and polysaccharide-conjugated vaccines based on the capsules of serotypes A, C, Y and W. An advantage of conjugate vaccines is their ability to generate an immunological memory. Due to similarities with the neural cell adhesive molecule, a human glycoprotein, the serogroup B capsule is poorly immunogenic as an antigen. Vaccines against serogroup B are based on surface proteins of Neisseria meningitidis group B.
The following meningococcal vaccines are approved for use in the EU based on a centralised licensing procedure:
- Menveo® (meningococcal groups A, C, W-135 and Y conjugate vaccine) is indicated for the immunisation of children from two years of age, adolescents and adults at risk of exposure to Neisseria meningitidis groups A, C, W-135 and Y to prevent invasive disease.
- Nimenrix® (meningococcal groups A, C, W-135 and Y conjugate vaccine) is indicated for the immunisation of individuals from the age of six weeks against IMD caused by Neisseria meningitidis groups A, C, W-135 and Y.
- Bexsero® (meningococcal group B surface protein vaccine) is indicated to protect individuals from the age of two months against IMD caused by Neisseria meningitidis serogroup B.
- Trumemba® (meningococcal group B surface protein vaccine) is indicated for active immunisation of individuals 10 years and older to prevent IMD caused by Neisseria meningitidis serogroup B.
Other meningococcal vaccines, such as meningococcal serogroup C conjugate vaccines, meningococcal A polysaccharide vaccines, meningococcal groups A, C, W-135 and Y polysaccharide vaccine and one combination vaccine with a Haemophilus influenzae B (Hib) component have been licensed by national health authorities in their respective Member States.
Disclaimer: The information contained in this factsheet is intended for the purpose of general information and should not substitute individual expert advice or judgement of healthcare professionals.