EU case definition
Creutzfeldt Jakob Disease (vCJD)
The legal basis, rationale and purposes of the EU case definitions can be found here.
The EU case definition for variant Creutzfeldt Jakob Disease (vCJD) is the following:
Preconditions
- Any person with a progressive neuropsychiatric disorder with a duration of illness of at least six months
- Routine investigations do not suggest an alternative diagnosis
- No history of exposure to human pituitary hormones or human dura mater graft
- No evidence of a genetic form of transmissible spongiform encephalopathy
Clinical Criteria
Any person with at least four of the following five:
- Early psychiatric symptoms [3]
- Persistent painful sensory symptoms [4]
- Ataxia
- Myoclonus or chorea or dystonia
- Dementia
Diagnostic Criteria
Diagnostic criteria for case confirmation:
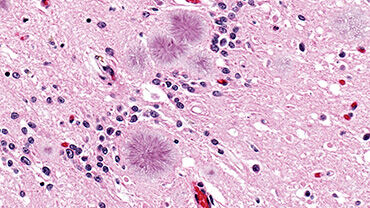
- Neuropathological confirmation: spongiform change and extensive prion protein deposition with florid plaques throughout the cerebrum and cerebellum
Diagnostic criteria for a probable or a possible case:
- EEG does not show the typical appearance [5] of sporadic CJD [6] in the early stages of the illness
- Bilateral pulvinar high signal on MRI brain scan
- A positive tonsil biopsy [7]
Epidemiological Criteria
An epidemiological link by human to human transmission (e.g. blood transfusion)
Case Classification
A. Possible case
Any person fulfilling the preconditions
AND
- meeting the clinical criteria
AND
- a negative EEG for sporadic CJD [8]
B. Probable case
Any person fulfilling the preconditions
AND
- meeting the clinical criteria
AND
- a negative EEG for sporadic CJD [9]
AND
- a positive MRI brain scan
OR
- any person fulfilling the preconditions
AND
- a positive tonsil biopsy
C. Confirmed case
Any person fulfilling the preconditions
AND
meeting the diagnostic criteria for case confirmation
( 3 ) Depression, anxiety, apathy, withdrawal, delusions.
( 4 ) This includes both frank pain and/or dysaesthesia.
( 5 ) The typical appearance of the EEG in sporadic CJD consists of generalised periodic complexes at approximately one per second. These may occasionally be seen in the late stages of vCJD.
( 6 ) See footnote 5.
( 7 ) Tonsil biopsy is not recommended routinely nor in cases with EEG appearances typical of sporadic CJD, but may be useful in suspect cases in which the clinical features are compatible with vCJD and MRI does not show pulvinar high signal.
( 8 ) See footnote 5.
( 9 ) See footnote 5.
Reference
Commission Implementing Decision 2012/506/EU of 8 August 2012, amending Decision 2002/253/EC laying down case definitions for reporting communicable diseases to the Community network under Decision No 2119/98/EC of the European Parliament and of the Council.
Other forms of Creutzfeldt Jakob Disease (vCJD)
ECDC coordinates the surveillance of communicable diseases across Europe under a legal framework, including Decisions 2119/98 and 2000/96. Under this framework, EU/EEA Member States are obliged to report on cases of vCJD using the agreed standard case definition.
Other forms of CJD are not explicitly included in the EU legal framework, and hence no formal EU case definitions exist. However these diseases are of public health importance, and differential diagnosis requires that other forms of CJD are considered when a diagnosis of vCJD is suspected. For this reason, summarised case definitions of other forms of CJD (Sporadic, Iatrogenic (Accidentally Transmitted) and Familial (Genetic)) are included below:
2.1 SPORADIC CJD
(from 1 January 2017)
|
1.1. DEFINITE: Progressive neurological syndrome AND Neuropathologically OR immunocytochemically OR biochemically confirmed 1.2 PROBABLE: 1.2.1 I + two of II and typical EEG* OR 1.2.2 I + two of II and typical MRI brain scan** OR 1.2.3 I + two of II and positive CSF 14-3-3 OR 1.2.4 Progressive neurological syndrome and positive RT-QuIC in CSF or other tissues 1.3 POSSIBLE: I + two of II + duration <2 years |
|
2.2. IATROGENIC CJD
|
2.2.1 DEFINITE Definite CJD with a recognised iatrogenic risk factor (see right) 2.2.2 PROBABLE 2.2.2.1 Progressive predominant cerebellar syndrome in human pituitary hormone recipients 2.2.2.2 Probable CJD with recognised iatrogenic risk factor (see right) |
RELEVANT EXPOSURE RISKS FOR THE CLASSIFICATION AS IATROGENIC CJD The relevance of any exposure to disease causation must take into account the timing of the exposure in relation to disease onset
This list is provisional as previously unrecognised mechanisms of human prion disease may occur |
2.3. FAMILIAL CJD/TSE (GENETIC)
|
2.3.1 DEFINITE 2.3.1.1 Definite TSE + definite or probable TSE in 1st degree relative 2.3.1.2 Definite TSE with a pathogenic PRNP mutation (see right) 2.3.2 PROBABLE 2.3.2.1 Progressive neuropsychiatric disorder + definite or probable TSE in 1st degree relative 2.3.2.2 Progressive neuropsychiatric disorder + pathogenic PRNP mutation (see right) |
P102L, P105L, A117V, G131V, F198S, D202N, Q212P, Q217R, M232T, 192 bpi
D178N129V, V180I, V180I+M232R, T183A, T188A, E196K, E200K, V203I, R208H, V210I, E211Q, M232R, 96 bpi, 120 bpi, 144 bpi, 168 bpi, 48 bp del
D178N129M
Y145s
H187R, 216 bpi,
I138M, G142S, Q160S, T188K, M232R, 24 bpi, 48 bpi, 48 bpi + nucleotide substitution in other octapeptides |
Additional list of mutations:
| PRNP MUTATIONS WITHOUT CLINICAL AND NEUROPATHOLOGICAL DATA | T188R, P238S |
| PRNP POLYMORPHISMS WITH ESTABLISHED INFLUENCE ON PHENOTYPE | M129V |
| PRNP POLYMORPHISMS WITH SUGGESTED INFLUENCE ON PHENOTYPE | N171S, E219K, 24 bp deletion |
| PRNP POLYMORPHISMS WITHOUT ESTABLISHED INFLUENCE ON PHENOTYPE | P68P, A117A, G124G, V161V, N173N, H177H, T188T, D202D, Q212Q, R228R, S230S |