Core protocol for ECDC studies of vaccine effectiveness against symptomatic laboratory-confirmed influenza or SARS-CoV-2 infection at primary care level
This document presents the core protocol for ECDC studies of CVE and IVE against symptomatic laboratory-confirmed influenza or SARS-CoV-2 infection, respectively, at primary care level. This core protocol presents the main elements for a multicentre (multi-country) study of IVE/CVE at primary care level, outlining the agreed methods for collecting data related to influenza and SARS-CoV-2 at country level, and includes a plan for the pooled analysis. The combination of data from multiple study sites will allow for studies with more statistical power to meet more specific objectives. The protocol can be implemented for COVID-19 and/or influenza.
Executive summary
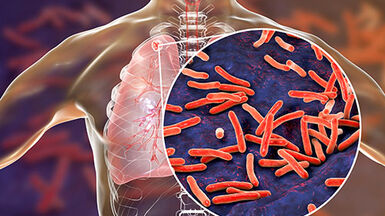
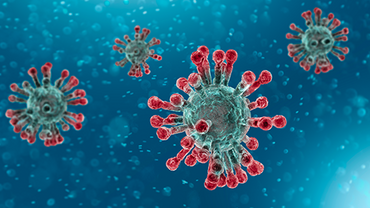
The end of 2019 saw the emergence of a novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) causing coronavirus disease 2019 (COVID-19). As of August 2023, eight vaccines had been authorised by the European Commission based on the scientific opinion of the European Medicines Agency (EMA) for use in the European Union (EU): Bimervax (previously COVID-19 Vaccine HIPRA), Comirnaty, COVID-19 Vaccine Valneva, Jcovden (previously COVID-19 Vaccine Janssen), Nuvaxovid (previously Novavax), Spikevax (previously COVID-19 Vaccine Moderna), Vaxzevria (previously COVID-19 Vaccine AstraZeneca), and VidPrevtyn Beta (indicated as a booster). In addition, four adapted vaccines have also been authorised: Comirnaty Original/Omicron BA.1, Comirnaty Original/Omicron BA.4-5, Spikevax bivalent Original/Omicron BA.1, and Spikevax bivalent Original/Omicron BA.4-5. Many other vaccines are under rolling review.
Influenza viruses undergo frequent genetic and antigenic changes. The influenza vaccine is reformulated each year and annual re-vaccination is recommended. Observed influenza vaccine effectiveness (IVE) varies from year to year between population sub-groups (age groups, risk groups) and differs for the various influenza types, subtypes and genetic clades, and outcomes measured. Immunological correlates of protection are not well defined. In 2017, the European Medicines Agency (EMA) formally adopted new guidelines on influenza vaccines covering, inter alia, post-authorisation studies of vaccine effectiveness, including brand-specific IVE data.
There is variation among the available influenza vaccine products currently in use for EU/EEA immunisation programmes, the target groups for vaccination, and the vaccination coverage across countries. New vaccines are
being developed for which limited or no effectiveness data are yet available in the EU. A comparison by vaccine type (adjuvanted vs nonadjuvanted, live attenuated vs inactivated, egg- vs cell-based), group (split virion, subunit, etc.)
and product could provide essential information for vaccine recommendations and health economic assessments.
In 2020, the European Commission stressed the importance of continuously monitoring the safety and effectiveness of vaccines in the EU/EEA in the post-authorisation phase, with particular emphasis on COVID-19 vaccines in the context of the ongoing pandemic. The 2018 ‘Council Recommendation on Strengthened Cooperation against Vaccine-preventable Diseases’ already called on ECDC and EMA to cooperate to ensure the continued monitoring of vaccines and vaccination in use in EU/EEA vaccination programmes. This request was subsequently formalised as part of the extended EMA regulatory mandate and ECDC’s newly amended mandate, requiring the two agencies to develop a structured and independent post-authorisation vaccine monitoring platform, initially prioritising COVID-19 vaccines. ECDC and EMA officially established and launched the platform in May 2022, with the intention of bringing together public health and regulatory experts to discuss the studies needed to generate real-life evidence on the safety and effectiveness of vaccines in use in EU/EEA immunisation programmes.
From 2020, ECDC began building infrastructure to perform COVID-19 vaccine effectiveness (CVE) studies using the lessons learned from other vaccine effectiveness studies. One such study was the ECDC-funded project I-MOVE (Influenza – Monitoring Vaccine Effectiveness in Europe), under which IVE was measured in Europe using primary care sentinel surveillance systems since the 2007–2008 influenza season. The infrastructure will be used to build a system that regularly monitors vaccine effectiveness and performs studies, including impact and burden of disease studies, in different settings. Depending on the setting, information will be provided on different outcomes (severe disease, moderate disease, transmission, etc). The overall project is called VEBIS (Vaccine Effectiveness, Burden and Impact Studies) and it includes different networks of study sites/countries/infrastructures, where the multi-country studies are conducted.
This document presents the core protocol for ECDC studies of CVE and IVE against symptomatic laboratory confirmed influenza or SARS-CoV-2 infection, respectively, at primary care level. This core protocol presents the main elements for a multicentre (multi-country) study of IVE/CVE at primary care level, outlining the agreed methods for collecting data related to influenza and SARS-CoV-2 at country level, and includes a plan for the pooled analysis. The combination of data from multiple study sites will allow for studies with more statistical power to meet more specific objectives. The protocol can be implemented for COVID-19 and/or influenza.
The proposed method is a case-control study using a test negative design. The study population consists of people of all ages, belonging to the target group for COVID-19 or influenza vaccination, presenting to primary care with
symptoms of acute respiratory infection (ARI) or influenza-like illness (ILI), and no contraindication for being vaccinated with the vaccine of interest. This protocol is adapted from the I-MOVE and I-MOVE+ generic protocols and the I-MOVE-COVID-19 generic protocol and is written in a generic manner. The specificities of each study site’s influenza and/or COVID-19 VE study can be detailed in the individual site protocol annexes (Annex 5).
This core protocol is primarily intended to guide the implementation of ECDC-funded studies. However, ECDC encourages the conduct of vaccine effectiveness studies, using this protocol as a basis, in countries not currently
planning to participate in ECDC-funded studies. The use of consistent protocols will facilitate the comparability of study results across studies, countries, and study sites.
This document presents version 1.0 of the core protocol which is an evolving document. This document will be updated and revised as necessary.