Reported decrease in antibiotic consumption across EU/EEA during COVID-19 pandemic
The latest data from the European Centre for Disease Prevention and Control (ECDC) show a decrease in the total antibiotic consumption in humans by more than 15% between 2019 and 2020. This has been seen in most EU/EEA countries, mostly in primary care, and most likely as a result of the COVID-19 pandemic. Nevertheless, antimicrobial resistance (AMR) levels remain high for several important combinations of bacterial species and antimicrobial groups, with the highest percentages generally reported by countries in the south and east of Europe.
“Antimicrobial resistance remains a serious challenge globally,” said Stella Kyriakides, EU Commissioner for Health and Food Safety. “Antimicrobial resistance is a silent pandemic that is happening here and now. Although antibiotic consumption generally decreased during the pandemic in the EU//EEA, we must increase our public health response. In the EU, we are stepping up our actions and have made the fight against AMR a priority. This includes actions under our Pharmaceutical Strategy, the legislation on veterinary medicines and medicated feed and the new Health Emergency Preparedness and Response Authority, HERA. Lives are lost because medicines no longer work and we need to step up global action, urgently. Investing in health today saves lives tomorrow”.
“Despite the focus on the ongoing pandemic, we need to keep up our efforts to further reduce unnecessary antibiotic use,” said Andrea Ammon, ECDC Director. “We also need to improve infection prevention and control practices in hospitals and other healthcare settings to significantly reduce the spread of antimicrobial-resistant bacteria. And in the primary care sector, many infections can be prevented through vaccination, respiratory etiquette, physical distancing and hand hygiene, thus potentially contributing to a decreased need to use antibiotics.”
The decrease in antibiotic consumption occurred mostly in the primary care sector and may be the result of a decrease in the number of primary care consultations, either because of hesitancy to seek healthcare for mild self-limiting infections, or difficulties in obtaining an appointment for a consultation. This has most likely resulted in fewer antibiotic prescriptions for mild and self-limiting infections and has had a more noticeable effect in countries where overuse and inappropriate use was common before the COVID-19 pandemic. It may also result from the reported low incidence of non-COVID-19-related respiratory tract infections in the EU/EEA in 2020, a likely consequence of the many non-pharmaceutical interventions, e.g. physical distancing, lockdowns, respiratory etiquette, use of face masks and promotion of hand hygiene, put in place as a response to the pandemic.
The large decrease in the consumption of antibiotics used to treat respiratory infections in the community in EU/EEA countries in 2020 is in line with both hypotheses. In the hospital sector, there was a decrease in antimicrobial consumption between 2019 and 2020 in about two-thirds of countries and an increase in the remaining EU/EEA countries that reported data.
“Although a decrease in antibiotic consumption has been seen in the EU/EEA countries, preliminary findings from the eastern part of the WHO European Region and Central Asia indicate that over time, antibiotic use rose. We know that access to antibiotics is a great concern, that over-the-counter sales still occur in parts of the European Region, that the antibiotics available are often the ones associated with the highest risk of developing resistance. COVID-19 is forcing us to fight health threats on multiple fronts, simultaneously. And AMR is among the gravest of challenges," said Dr Hans Henri P. Kluge, WHO Regional Director for Europe.
Concerning antimicrobial resistance levels, more than half of the Escherichia coli isolates reported to ECDC, and more than a third of the Klebsiella pneumoniae isolates, were resistant to at least one antimicrobial group under surveillance, and combined resistance to several antimicrobial groups was frequent. Carbapenem resistance was common in P. aeruginosa and Acinetobacter species. There was also an increasing trend in the percentage of vancomycin-resistant isolates of E. faecium in the EU/EEA, which increased from 11.6% in 2016 to 16.8% in 2020.
Resistance to last-line antibiotics such as vancomycin and those in the carbapenems group remains a major issue. When these antibiotics are no longer effective, there are very limited treatment options that may not work in all situations, sometimes leading to fatal outcomes. Resistance to last-line antibiotics also compromises the effectiveness of life-saving medical interventions such as cancer treatment and organ transplantation.
NOTES TO EDITOR
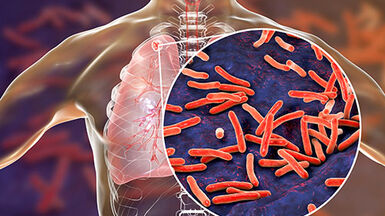
- ECDC estimates that each year, more than 670 000 infections occur in the EU/EEA due to bacterial resistance to antibiotics and that approximately 33 000 people die as a direct consequence of these infections. The health burden of antimicrobial resistance is comparable to that of influenza, tuberculosis and HIV/AIDS combined.
- Klebsiella pneumoniae is a common cause of urinary tract, respiratory tract and bloodstream infections and is a frequent cause of hospital outbreaks if appropriate prevention and control measures are not taken. Very few therapeutic options remain available for patients infected with multidrug-resistant K. pneumoniae with additional resistance to carbapenems and are often limited to combination therapy and older antibiotics, such as colistin, an antibiotic from the polymyxins group.
- Escherichia coli is one of the most frequent causes of bloodstream infections and community- and healthcare-associated urinary tract infections worldwide.
- Pseudomonas aeruginosa and Acinetobacter species cause healthcare-associated infections and often result in hospital outbreaks if appropriate prevention and control measures are not implemented. They can persist in the healthcare environment and are difficult to eradicate once established.
- Vancomycin-resistant Enterococcus faecium has been listed by the World Health Organization as a pathogen with high priority in its global priority list of antibiotic-resistant bacteria, emphasising the paucity of available and effective treatment options. High levels of antimicrobial-resistant enterococci remain a major infection control challenge and an important cause of healthcare-associated infections in Europe. In addition to the fact that infections caused by resistant strains are difficult to treat, enterococci are easily disseminated in healthcare settings.
European Antibiotic Awareness Day
European Antibiotic Awareness Day (EAAD) is a European health initiative coordinated by ECDC, which provides a platform and support for national campaigns on the prudent use of antibiotics. Each year, EAAD is marked by national campaigns on or around 18 November. Prudent use means only using antibiotics when they are needed, with the correct dose, dosage intervals and duration of the course. Please visit http://antibiotic.ecdc.europa.eu for more information and follow the discussion on social media. Follow the hashtags #EAAD #AntibioticResistance #KeepAntibioticsWorking