Infectious disease surveillance summary, 2014 data
Suggested citation: European Centre for Disease Prevention and Control. Annual Epidemiological Report 2016 – Infectious disease surveillance summary, EU/EEA, 2014 data. [Internet]. Stockholm: ECDC; 2016 [cited YYYY Month DD]. Available from: https://ecdc.europa.eu/en/infectious-diseases-public-health/surveillanc…
Infectious disease surveillance is an imperfect art, fraught with inherent limitations such as underdiagnosis, underreporting and various reporting biases. Disease surveillance in the EU/EEA faces the additional challenge of widely heterogeneous national surveillance systems reporting to the European level, which may compromise data comparability across Member States. Within these constraints, however, a number of reasonably justified conclusions can be drawn from the EU/EEA infectious disease surveillance data collected for 2014 and presented in the ECDC Annual Epidemiological Report.
Among the notifiable diseases under comprehensive case-based surveillance, the most commonly reported in 2014 were, in descending order, chlamydia infection, campylobacteriosis, salmonellosis, gonorrhoea and tuberculosis. These diseases accounted for just over 850 000 cases, 75% of the 1.1 million reported cases of notifiable infectious diseases in the EU/EEA in 2014. The highest numbers of deaths were reported for tuberculosis (n=4 279) and HIV/AIDS (n=1 131), followed by invasive pneumococcal disease (n=713), Legionnaires’ disease (n=456) and listeriosis (n=210). As high as these morbidity and mortality figures may seem, they are put into perspective by EU/EEA excess all-cause mortality estimates of over 200 000 deaths in people 65 years of age and older during the 2014–15 influenza season, which was dominated by subtype A(H3N2) and aggravated by a poorly effective seasonal vaccine.
Food- and waterborne diseases
Of the seven priority food- and waterborne diseases under enhanced EU/EEA surveillance, campylobacteriosis and yersiniosis showed no clear trend in notification rate between 2010 and 2014. Two of the potentially more severe diseases, listeriosis and Shiga-toxin-producing Escherichia coli (STEC) infection, saw an increasing trend in notifications. EU/EEA surveillance of listeriosis is known to be biased towards severe cases, which are especially common among the elderly. The increase observed may thus partly reflect the ageing population in many Member States. STEC surveillance is likely to have benefitted from improved clinical and laboratory awareness following the large outbreak in 2011 (which mainly involved German cases) and from the increasing use of diagnostics based on polymerase chain reaction. The remaining three food- and waterborne diseases under enhanced EU/EEA surveillance (non-typhoidal salmonellosis, typhoid and paratyphoid fever, and shigellosis) showed decreasing trends, most likely attributable to the implementation of Salmonella control programmes in the poultry industry, improved personal hygiene and – for typhoid and paratyphoid fever and shigellosis – changing travel patterns.
A large hepatitis A outbreak associated with the consumption of mixed frozen berries, involving cases in several EU/EEA countries and first detected in 2013, lasted well into 2014. Finally, Legionnaires’ disease continued its increasing trend observed since 2011 and, in 2014, reached the highest rate hitherto recorded, which was partly explained by a large community outbreak near Lisbon.
Sexually transmitted diseases
The notification rates for chlamydia infection appear to be stable, but are known to reflect testing practices rather than the epidemiology of the disease. The rates for gonorrhoea, syphilis and lymphogranuloma venereum all showed increasing trends between 2010 and 2014, largely driven by infections among men who have sex with men (MSM).
The overall HIV notification rate has been stable since 2005. However, during the same period, the number and proportion of MSM among newly diagnosed HIV cases has increased markedly, as opposed to all other at-risk subpopulations, which showed a decrease in the percentage of cases.
Hepatitis B and C notifications remain challenging to interpret. Both rates seem to increase, but the vast majority of cases are known (hepatitis B) or suspected (hepatitis C) to be newly diagnosed chronic cases. It is therefore unclear to what extent this is a consequence of increased testing in the few countries reporting the most cases. The most common route of transmission reported for acute cases of hepatitis B in 2014 was heterosexual contact; for hepatitis C it was injecting drug use. For both infections, the second most commonly reported route of transmission for acute cases was nosocomial. Five countries accounted for the overwhelming majority of nosocomially infected cases, which may be partly due to the high prevalence of hepatitis B and C in the general population and suboptimal hospital infection control in these five countries, but may also result from underreporting of nosocomial transmission in some of the other countries. The declining long-term trend in acute cases of hepatitis B is likely to be attributable to universal childhood vaccination in most Member States.
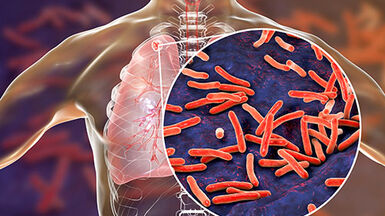
Tuberculosis
Although still substantial, tuberculosis morbidity and mortality in the EU/EEA has been steadily decreasing for many years and continued to do so in 2014. Multidrug resistance remained stable at 4% of the mycobacterial isolates tested.
Vaccine-preventable diseases
Pertussis and invasive pneumococcal disease accounted for over 50% of all notified cases of vaccine-preventable diseases (VPD) and over 60% of VPD-related deaths in 2014, not counting influenza. The notification rate of pertussis has increased in recent years despite sustained high vaccination coverage, most likely a result of improved awareness by clinicians, better diagnostics, waning immunity, and changes in circulating strains. Invasive pneumococcal disease has shown a decreasing trend, but there is a growing proportion of cases caused by serotypes that are not included in the currently licensed conjugate vaccines.
Compared with previous years, the number of measles cases reported in the EU/EEA in 2014 was low. This must be largely due to the reduced number of susceptible individuals after several large outbreaks, as vaccination coverage for the second dose of measles vaccine in 20 Member States was below the 95% minimum coverage threshold recommended by WHO.
Emerging and vector-borne diseases
The year 2014 marked the first documented outbreak of Ebola virus disease in West Africa and the largest epidemic of its kind ever, with close to 30 000 notified cases and over 11 000 deaths, including many occupational deaths in healthcare workers. Despite the unprecedented size of this outbreak in Africa, only eight cases of Ebola disease were notified in the EU/EEA in 2014.
Most emerging and vector-borne diseases under surveillance remained at a low level in 2014 but cases of chikungunya fever increased 20 times (compared with 2013 levels) to over 1 400 cases. The majority of cases were related to travel to the Caribbean and the Americas, where a large outbreak was ongoing at that time.
Eleven autochthonous cases of chikungunya fever notified in southern France serve as a reminder that, with a competent vector present in parts of Europe, it may only take one imported case to trigger a chain of local transmission.
Healthcare-associated infections
Just as previous years, 2014 was characterised by frequent reports of surgical site infections and healthcare-associated infections in patients admitted to an intensive care unit (ICU) for more than two days. These notifications, however, are only one part of the picture because about half of the Member States did not participate in these two EU/EEA surveillance schemes, and even among participating hospitals, reputational concerns may have posed an inherent disincentive to comprehensively report all cases.
The majority of cases in ICUs were reported as pneumonia due to intubation. Device-adjusted infection rates of ICU-acquired pneumonia, bloodstream and urinary tract infections remained stable compared with 2012. The most commonly reported surgical site infections were those following colon surgery, but their in-hospital incidence density showed a decreasing trend between 2011 and 2014. Surgical site infections following coronary artery bypass grafts and knee replacements also declined whereas the cumulative incidence of infections following cholecystectomy increased.
Antimicrobial resistance
Earlier trends in antimicrobial resistance in common bacteria that cause invasive infections continued in 2014. This meant a further decrease of meticillin-resistant Staphylococcus aureus, but also increasing trends of resistance in gram-negative bacteria, including multidrug resistance and resistance to last-line drugs like carbapenems and, in certain parts of Europe, polymyxins. Pre-existing geographic trends also persisted in 2014, with lower resistance percentages generally reported by countries in the north and higher resistance percentages in the south and east of Europe. This is most likely related to differences in antimicrobial use, infection control and healthcare utilisation practices.
Public health actions
A number of possible public health actions can be derived from the 2014 EU/EEA infectious disease surveillance data:
- ECDC and the Member States should continue to improve the timeliness, quality and comparability of surveillance data across the EU/EEA to make them an even more useful source of relevant information for action.
- Even though EU/EEA surveillance data may not be entirely comparable across Member States, differences in disease rates between countries suggest that some national prevention and control strategies are more effective than others. This should inspire efforts to learn from the most successful models.
- Control programmes targeting certain Salmonella serovars in the poultry industry seem to have had a positive effect on the epidemiology of human salmonellosis. European policymakers may consider similar programmes for Salmonella serovars that have not been targeted in the past, and, at the same time, expand control programmes to other branches of the food industry.
- Current strategies to prevent HIV and other sexually transmitted infections among MSM do not appear to be sufficiently effective, so relevant national efforts should be intensified or redesigned to meet their purpose
- More effective influenza vaccines should be developed which might also boost vaccine uptake, including in those groups most at risk.
- New pertussis vaccines should confer longer-lasting immunity. Alternatively, pertussis vaccination schedules should consider adolescent and adult boosters as well as vaccinations for healthcare workers and pregnant women.
- To eliminate measles, the 20 Member States with insufficient vaccination coverage may want to consider more active measures to close their immunisation gaps by addressing vaccination hesitancy among parents and healthcare workers and raising awareness among politicians
- Despite considerable progress in some parts of the EU/EEA, prudent antimicrobial use and comprehensive infection prevention and control strategies should continue to be rigorously enforced across all healthcare sectors to prevent selection and transmission of antimicrobial-resistant bacteria (ECDC directory of online resources).
In an area as diverse as the EU/EEA, some of these suggestions may be more relevant to some countries than others. Yet, with infectious diseases, anything that is allowed to fester in one place for too long may sooner or later also affect the neighbourhood. In this sense, disease surveillance and, ultimately, successful prevention and control, can only be obtained through collective efforts across administrative borders, building on sound common priorities, common standards, and the frequent exchange of knowledge and best practices.